COPD
Manchester's Premier Respiratory Clinic
What is COPD?
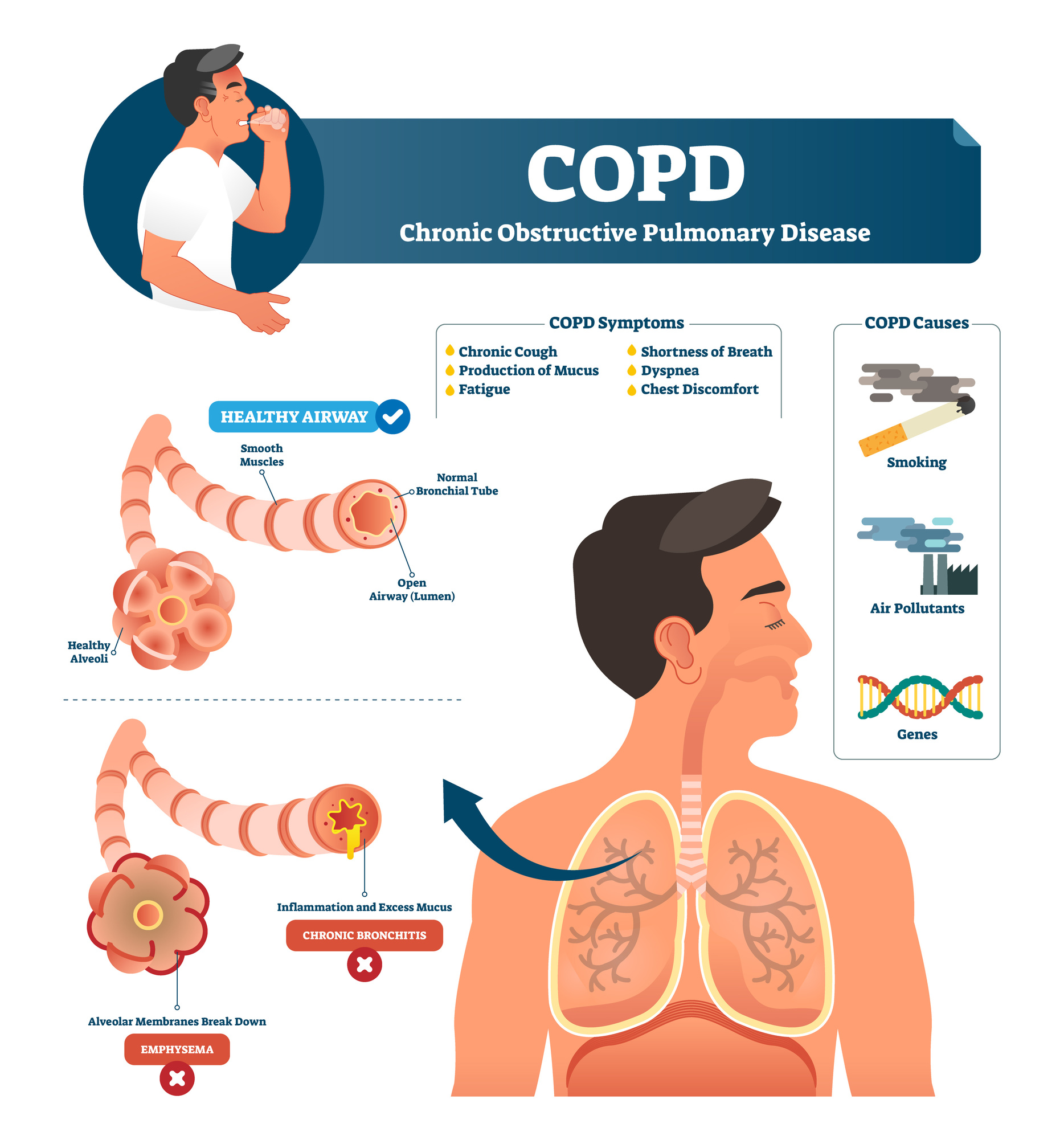
Chronic Obstructive Pulmonary Disease consists of 2 disease pathologies:
- Emphysema where the architecture of the lung is damaged leading to collapsibility of the airways and destruction of the alveoli, which is the part of the lung which we rely on to exchange oxygen from the atmosphere in to our body.
- Chronic bronchitis is a process where inflammation within the lung’s airways leads to loss of structural integrity with in the airways leading to airway narrowing. There is also increase of mucus production which leads to plugging of the airways adversely impacting on the flow of air and gas exchange. The increased mucus production also increases the risk of recurrent respiratory infections and often the airways become chronically infected by bacteria.
The term COPD defines the predominant process that is a long standing (Chronic) and causes narrowing of the airways making it difficult to breathe especially on expiration. Although the disease primarily affects the lungs, the severity, infective nature and chronicity of the process leads to symptoms which impact on other parts of the body (see section on associated symptoms).
Symptoms
Symptoms often only appear when significant lung damage has occurred and from then on there is steady progression, punctuated by rapid deteriorations related to increasingly occurring lung infections.
COPD presents with lung as well as more general symptoms:
- Shortness of breath, especially during physical activities
- Wheezing, on expiration with prolongation of the time it takes to breath out due to increased collapsibility of the airways.
- Chest tightness which gets worse as the breathlessness progresses
- A chronic cough productive of mucus (sputum). Increased mucus production leads to an increased risk of recurrent chest infections.
- Frequent respiratory infections also referred to as exacerbations. Exacerbations can be infective with bacterial or viral causes, though some exacerbations can be non-infective.
- Lack of energy, due to increased work of breathing and progressive loss of muscle strength
- Unintended weight loss (in later stages) also known as respiratory cachexia, as the disease progresses the work of breathing is greater then the calorie intake leading weight loss.
- Swelling in ankles, feet or legs, this is a sign of severe disease with the presence of low levels of body oxygenation leading to a strain on the heart.
- Anxiety and depression, is common in patients’ with chronic lung disease. The causes of the psychology impact in COPD are multiple including: progressive limitation in exercise capability leading to social isolation and dependency on others, recurrent exacerbations causing severe often life threatening episodes, chronic infections leading to malaise etc
Causes
- SMOKING: The most significant risk factor for COPD is long-term cigarette smoking. The more years you smoke the greater your risk. Pipe smokers, cigar smokers and marijuana, illicit drug smokers, as well as people exposed to large amounts of secondhand smoke are all at risk.
- OCCUPATIONAL EXPOSURES: To dusts and chemicals. Long-term exposure to chemical fumes, vapours and dusts in the workplace can irritate and inflame your lungs.
- GENETICS: The uncommon genetic disorder alpha-1-antitrypsin deficiency is the cause of some cases of COPD, usually in the presence of cigarette smoking exposure.
Diagnosis
Diagnosis is based on a consultation with your doctor. The history taken with an examination helps confirm the likely cause of symptoms, which then supports the most effective investigation pathway to corroborate the diagnosis and severity of the underlying condition.
LUNG FUNCTION TESTS:
Are blowing tests that assess the ability of the lungs to move air in and out of the lungs as well as assessing the volume of the lungs and its ability to transfer oxygen in the air in to the blood to support oxygenation of the body.
RADIOLOGY:
- A chest X-ray can show emphysema, one of the main causes of COPD. An X-ray can also rule out other lung problems or heart failure.
- A CT scan of your lungs can help detect emphysema and help determine if you might benefit from surgery for COPD. CT scans can also be used to screen for lung cancer.
ARTERIAL BLOOD GASES:
- This blood test measures how well your lungs are at transferring oxygen into your blood and removing carbon dioxide.
Treatments
Inhalers:
- Short acting bronchodilators: act to open up the airways and often are the first line of treatment to support exertional breathlessness in the early phase of the disease. The impact of the medication lasts for around 4 hours and is used before exercise to allow individuals to walk further or to support symptoms of breathlessness, wheeze and / or chest tightness.
- Long acting bronchodilators: These inhalers open up the lung for a longer period (12 to 24 hours) and aim to improve day to day functioning and also they have been shown to reduce exacerbations.
- Inhaled corticosteroids: These inhalers are used in combination with Long acting bronchodilators to reduces exacerbations (‘lung flare ups’) and improve quality of life and functioning in individuals with COPD.
Oral Medication:
- Mucolytics: These are medications that reduce sputum production and hence are used to reduce infections. The reduction of mucus also will reduce the severity of coughing.
- Oral Steroids: These are used to treat the acute inflammation related to exacerbations and in some patients with progressed disease a maintenance dose can be used but the side effects of long term oral steroids needs to be balanced with the benefits in patients.
- Antibiotics: In most patients with COPD antibiotics are used to treat acute infective exacerbations by the GP. Individuals who have frequent exacerbations can be given rescue medications to keep at home to aid the time from infection onset to treatment.
- Theophylline tablets: is a type of bronchodilator. It's unclear exactly how theophylline works, but it seems to reduce swelling (inflammation) in the airways and relax the muscles lining them. Possible side effects include:
- feeling and being sick
- headaches
- difficulty sleeping
- noticeable pounding, fluttering or irregular heartbeats
Other Treatment Options
Oxygen: Oxygen therapy is given in patients who demonstrate reduction in oxygen concentration in their blood severe enough to cause heart strain. There are 2 forms of oxygen delivery:
- Long term Oxygen therapy (LTOT): this is given via nasal cannula for a minimum of 16 hours a day.
- Ambulatory Oxygen: This allows patients whose oxygen levels fall very low during exertion to use small canisters of oxygen whilst walking to improve daily activity.
Oxygen is not provided to improve breathlessness in individuals where critical desaturation does not occur.
Surgery
Surgery and specialist bronchoscopic technique can be used to reduce overinflated lungs in certain patients. The process is really only applicable where lung volume re-education surgery supports the reflation of ‘squashed’ healthy lung.
Lung Transplantation is an option for a few patients who have less than 2 years to live and provision of a replacement lung may improve quality of life.

